This information HAS errors and is made available
WITHOUT ANY WARRANTY OF ANY KIND and without even the
implied warranty of MERCHANTABILITY or FITNESS FOR A
PARTICULAR PURPOSE. It is not permissible to be read by
anyone who has ever met a lawyer or attorney. Use is confined to
Engineers with more than 370 course hours of engineering.
If you see an error contact:
+1(785) 841 3089
inform@xtronics.com
"The LPA gene that codes for apo(a) evolved from plasminogen in
Old World monkeys: high homology between apo(a) and plasminogen"
Working narrative - Lp(a) levels, like other lipoprotiens may or may not have anything to do with heart disease. It happens as a reaction to the damage of the intima - they have the arrow of causation reversed?
"The LPA gene that codes for apo(a) evolved from plasminogen in
Old World monkeys: high homology between apo(a) and
plasminogen"
This is a big hint - Thus, one could interpret the fact that
Lp(a) is a clotting factor that CVD is a thrombotic disease rather
than a disease of lipids.
The clots formed with LP(a) are much harder to be resorbed.
Everyone has some Lp(a)
The other important bit is the striations in plaque - which should
change the narrative of CVD.
https://pubmed.ncbi.nlm.nih.gov/36869878/
What is most likely what is going on are repeated clots - which
get paved over with new intima (similar to what happens to stents)
. These repeated clot layers eventually narrow the
artery.
Everyone has some Lp(a) . 80% of the public has some amount
of T2D from eating packaged foods. This translates into
chronically elevated insulin levels - insulin further prevents
resorption of plaque. Proper intervention for CVD would Seem
to warrant interventions to lower insulin - intermittent fasting (
only eat say 8 hours out of the day).
https://www.sciencedirect.com/science/article/pii/S0022227520309792
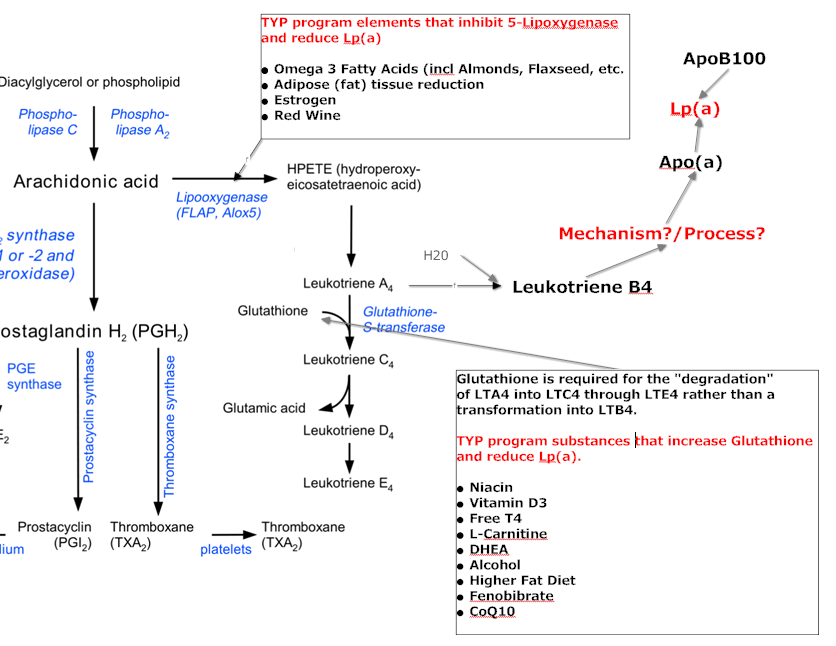
So IL-6 => Lp(a) ?
Lp(a) => Il-6 and Il-8
Can excess zinc increase apo(a)?
Leukotriene A4 hydrolase: A zinc metalloenzymeThis is not surprising - for APO(a) to bind to LDL there has to be a source of energy, so there is more to this that what is in these papers. First, oxLDL stimulates the intima wall and starts an immune response - my guess is that there is likely a messenger that tells the liver to make APO(a) which binds to LDL forming Lp(a). Lp(a) can be further oxidized into oxLp(a). (oxLDL can also be double oxidized - and I would guess the same for oxLp(a)).
Another way of thinking about this is Lp(a) is a kind of LDL so the LOX-1 receptor may also bind to oxLp(a).
So until Lp(a) becomes oxLp(a) would not say that Lp(a) is an oxLDL - Lp(a) is made up of apoB-100 linked by a sulfhydryl bond apo(a) of variable size(isoforms). This bond (See www.microbiologytext.com/index.php ) is a covalent bond between cysteine groups. My hunch is this bond's energy comes form the LDL being in the oxidized state - reducing the oxLDL to form Lp(a).
So it could be that APO(a) is protective, but my hunch is if one
has the wrong isoforms of Lp(a), then Lp(a) isn't protective - it
may actually make things very much worse. (It appears that APO(a)
is heterogeneous - individuals produce more than one isoform) But
we don't know for sure - this would make Lp(a) the smoke, not the
fire and makes me pause about the goal of reducing the level -
different interventions may use different methods to reduce Lp(a).
We know Niacin increases HDL - which carries antioxidants that can
reduce oxLDL - thus less irritation of the intima wall and less
messenger to the liver to produce APO(a) thus less Lp(a). Other
methods may interfere with the messanger - and this may be good or
bad. It may be that we want a drug that would target only the bad
isoforms of APO(a) and leave the good APO(a) alone.
Thus LDL => oxLDL + APO(a) =>oxLP(a) => oxoxLp(a)=> very bad outcomes.
oxLDL (as I keep saying) is central to the disease process - it integrates many things that we know - it has great explainative power. IMHO measuring oxLDL should be central in CVD treatment - particularly for people with elevated Lp(a).
The good news is we know some things that lower oxLDL
Apo(a) Inhibition of Plasminogen Activation
LP(a) appears with different isoforms of apolipoprotein - 40% of the variation in Lp(a) levels when measured in mg/dl can be attributed to different isoforms. Combine that with the lighter Lp(a) being more disease causing and a test in mg/dl is not useful.
Glutathione promoters:
IGF-I was found to lower Lp(a) by up to 60% (Atherosclerosis: diet and drugs By Arnold von Eckardstein)?
a combination with a fibrate (clofibrate) may work better than Niacin alone
Niacin essentially constitutes the nicotinamide ring, the reactive site of the NADP and NADPH molecule. Ascorbate reduces the NADP molecule to NADPH and thereby "recharges" the molecule for metabolic reactions. Niacin and ascorbate have also been shown to be effective in lowering elevated plasma levels of low-density lipoprotein (LDL) and very low-density lipoprotein (VLDL). Thus NADPH may also be involved in the regulation of other potentially atherogenic lipoproteins. Further confirmation of this therapeutic mechanism will establish the value of dietary niacin and ascorbate supplementation in reducing elevated plasma levels of atherogenic lipoproteins.
Should we be using IR Niacin? Not clear
testosterone alone and by 28% when testosterone and testolactone
were combined,...
I wonder if people realize that testosterone gets converted to
estrogen?
Next - is an older study in mass - needs to be redone in nmol
Clomid?
??
This study needs to be re-run using nmol
2 G?
These high doses of carnitine may lead to excess energy, restlessness, perhaps insomnia?
600 - 800mg? http://www.fasebj.org/content/15/13/2423.abstract
Mostly for people with high trygly? Or does reduction of LDL cause less Lp(a)? Lots of non replicated studies.
Sadly, the control for the above was rapeseed oil - which is 21% 18:2 ω-6 linoleic acid thought to increase LDL oxidation.
18.1% (95% CI -32.2, -3.9) decline in Lp(a) from baseline, but these declines did not significantly differ from women who received placebo.
DHEAS was negatively related to apolipoprotein A
Lp(a) reductions over 70% -- one small study. May be slight risk here - A human would have to take in 448,000 mg of NAC per day to = this level of mouse intake. - From:
NAC-treated mice developed pulmonary arterial hypertension (PAH) that mimicked the effects of chronic hypoxia.
Perhaps IGF-1( insulin-like growth factor–I) may reduce lipoprotein(a) levels.
Contrasting Effects of Growth Hormone and Insulin-Like Growth Factor–I}
According to Wikipiedia
IGF-1 in the circulation include an individual's genetic make-up, the time of day, his or her age, gender, exercise status, stress levels, nutrition level and body mass index (BMI), disease state, race, estrogen status and xenobiotic intake
More at:
There do appear to be some drugs that increase IGF-1 according to the Wiki article.. (Creatine? How much? blue berries? http://www.ncbi.nlm.nih.gov/pubmed/15682927 )
Fosinopril
This might be why thyroid optimization is important in CAD
Information is at About_Hypothyroidism
CQ10? 60mg BID
Apheresis is the most effective way of reducing lipoprotein a levels. Apheresis involves separating the blood externally to the body, so that the lipoprotein(a) may be effectively 'filtered out', and the blood is then returned back to the patient. This treatment is very expensive and generally only available to very high risk patients.
Systemic acetyl-L-carnitine elevates nigral levels of glutathione and GABA
www.ncbi.nlm.nih.gov/pubmed/15001526
This could explain why high BG seems causative of CVD - via Lox-1
www.springerlink.com/content/3b2ftmx3t5bjbr85/ journals.lww.com/jhypertension/Abstract/2005/01000/Cardioprotective_mechanisms_of_Rho_kinase.17.aspx
www.proteinkinase.biz/modules/GoShopping/article_images/Y27632.pdf atvb.ahajournals.org/cgi/content/abstract/23/12/2203 circ.ahajournals.org/cgi/content/abstract/circulationaha;100/9/899 ACE inhibitors block Angiotensin I => Angiotensin II conversion effect on Lp(a)? www.ncbi.nlm.nih.gov/pubmed/8285181 www.sciencedirect.com/science
ASA? cardiovascres.oxfordjournals.org/content/64/2/243.full circres.ahajournals.org/cgi/content/short/94/3/370 www.enzolifesciences.com/fileadmin/enzo/BML/EI395.pdf
What interleukin(s) increase or decrease Apo(a)?
ASA? http://www.ncbi.nlm.nih.gov/pubmed/10567380
IGF-I was found to lower Lp(a) by up to 60% (Atherosclerosis: diet and drugs
By Arnold von Eckardstein)?
Fosinopril ACE inhibitor lowers Lp(a)?
Fosinopril seems to be the only ACE inhibitor to reduce Lp(a) concentrations in non-proteinuric patients as well, probably by increasing apo(a) fragmentation and excretion into the urine (Kostner K et al., unpublished data). Other data limits this to kidney diseased?
I also found more than one article that shows that Human grow hormone may INCREASE Lp(a) while improving the overall lipid profile. Makes me question DHEA?
From Wiki
NADPH oxidase is a major cause of atherosclerosis, and NADPH oxidase inhibitors may reverse atherosclerosis. Atherosclerosis is caused by the accumulation of macrophages containing cholesterol (foam cells) in artery walls (in the intima). NADPH oxidase produces ROSs. These ROSs activate an enzyme that makes the macrophages adhere to the artery wall (by polymerizing actin fibers). This process is counterbalanced by NADPH oxidase inhibitors, and by antioxidants. An inbalance in favor of ROS produces atherosclerosis. In vitro studies have found that the NADPH oxidase inhibitors apocynin and diphenyleneiodonium, along with the antioxidants N-acetyl-cystine and resveratrol, depolymerized the actin, broke the adhesions and allowed foam cells to migrate out of the intima
This suggests that vit C will reduce Lp(a) and L-lysine and
L-proline may protect the arteries.:
It may be that Vit C helps because it converta proline to hydroxyproline.. The latest reference in this paper was 1992..
www.pubmedcentral.nih.gov/picrender.fcgi Evidence that the Fibrinogen Binding Domain of Apo(a) Is Outside the Lysine Binding Site of Kringle IV-10 A Study Involving Naturally Occurring Lysine Binding Defective Lipoprotein(a) Phenotypes
EACA decreased the binding of Lp(a) to PM-fibrinogen
Core of the Proteoglycan Decorin ]
So:
What dosage of L-lysine and L-proline would make sense?
What about apocynin ?
It appears that actone and Homocysteine thiolactone are related in
some way.. and Homocysteine is related to Osteoporosis. Vitamin D,
estrogen, actone, HGH, and testosterone all increase bone density
and might reduce Lp(a). This seems somehow linked to reducing
Lp(a).
| Top Page | wiki Index |